
Share Post:
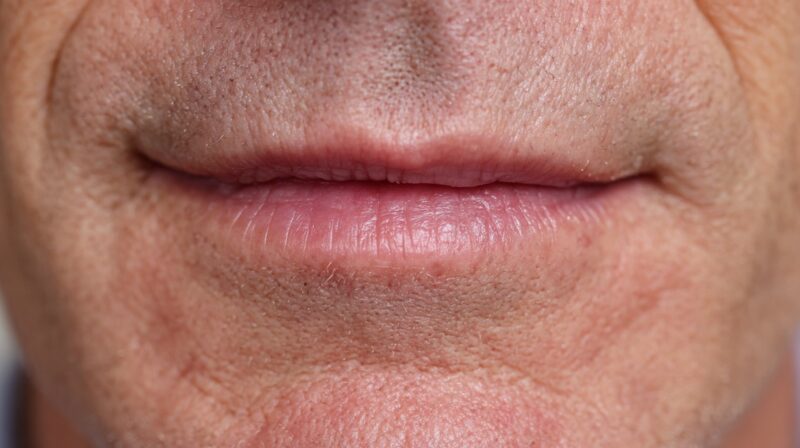
Dry mouth, medically known as xerostomia, often becomes more noticeable after age forty. Saliva plays a major role in oral comfort, dental protection, digestive support, and the overall feel of a healthy mouth.
Many adults reach midlife and start experiencing changes that make moisture levels drop, causing daily discomfort and new dental challenges.
A clear look at the causes and helpful strategies provides a practical way to control symptoms, protect oral health, and regain comfort.
Table of Contents
ToggleWhy Dry Mouth Becomes More Common After 40
Many adults start noticing a gradual shift in oral comfort as they pass their forties.
Saliva no longer flows as easily, and the mouth may feel dry, tight, or irritated throughout the day.
Multiple factors work together to create this change, including natural aging, shifting hormone levels, lifestyle habits, and common health conditions.
Greater awareness of these influences helps individuals find practical ways to restore moisture and improve daily comfort.
Physiological and Hormonal Changes
Many changes happen inside the body during midlife, and some of the most impactful involve hormonal fluctuations.
Salivary glands depend on stable hormone levels to function smoothly, so shifts create noticeable dryness.
People entering perimenopause or menopause often feel these effects strongly.
- Hormonal balance affects moisture regulation in the mouth.
- Estrogen fluctuations reduce saliva output and irritate oral tissues.
- Aging lowers salivary gland efficiency even without other medical influences.
Hormonal variation during perimenopause and menopause influences many internal systems, including salivary function.
Estrogen levels move up and down unpredictably, often reducing moisture in the mouth and throat.
Aging adds another layer of change, since salivary glands naturally produce less fluid as people grow older. Many adults notice dryness first at night or during conversations that last a long time.
Gradual shifts in gland function make dryness more frequent, lingering longer and causing more discomfort without active steps to control it.
Medication Side Effects

Many people in their forties and fifties begin using medications that unintentionally reduce saliva.
Saliva reduction often appears as a side effect rather than the primary purpose of the drug, yet the impact can feel strong and constant.
- Antidepressants
- Blood pressure medications
- Antihistamines
- Muscle relaxants
Many medications taken in midlife contribute to dryness because they limit saliva production. Increased use of multiple prescriptions, often called polypharmacy, raises the chance of significant dryness, especially when taken daily for long periods.
Additional prescriptions sometimes amplify dryness when their effects overlap.
Many individuals find relief after discussing options with their healthcare provider, since alternatives or dose adjustments can reduce dryness without compromising overall treatment.
Lifestyle Factors
Daily habits often influence moisture levels more than people realize.
Some behaviors make dryness more intense or more frequent, especially when combined with hormonal or medication effects.
- Smoking
- Alcohol consumption
- High caffeine intake
- Nighttime mouth breathing
- Snoring
Smoking irritates tissues inside the mouth and slows saliva flow. Alcohol creates a drying effect, especially during evening use or social drinking.
Caffeine increases fluid loss, which reduces moisture further. Mouth breathing quickly dries the mouth, particularly during sleep, and snoring intensifies airflow, making dryness more severe.
Small lifestyle changes often provide noticeable relief when dryness is mild or moderate.

Underlying Health Conditions
Chronic health conditions often interfere with saliva production and make midlife dryness more difficult to manage.
Some conditions affect the glands directly, while others impact the nervous system or immune system in ways that lower saliva output.
- Diabetes
- Autoimmune disorders such as Sjögren’s syndrome
- Alzheimer’s
- History of radiation or chemotherapy
Chronic conditions such as diabetes and autoimmune disorders often lower saliva levels by disrupting normal gland activity.
Cancer treatments such as chemotherapy or radiation may damage salivary glands and cause long-lasting dryness.
People diagnosed with these conditions frequently benefit from specialized dental care and medical guidance.
Symptoms and Consequences of Chronic Dry Mouth
Many people do not immediately realize that their symptoms come from reduced saliva.
Dryness progresses slowly, so early signs are often overlooked.
- Sticky or rough sensation
- Burning feeling on the tongue
- Cracked lips
- Persistent bad breath
- Sore throat
- Trouble chewing or swallowing
- Difficulty speaking comfortably
Dryness often feels like a sticky or rough texture inside the mouth. A burning sensation may develop on the tongue or cheeks, especially after eating salty or acidic foods.
Lips may crack more easily, and a sore throat can linger through the day.
Persistent bad breath appears when saliva cannot wash away bacteria effectively.
People with chronic dryness sometimes struggle to speak for long periods, swallow pills, or chew dry foods. Symptoms grow stronger as dryness becomes more constant.
Oral Health Risks
Insufficient saliva creates a long list of oral health complications because saliva normally protects teeth and gums.
- Higher risk of cavities
- Increased gum irritation
- More frequent oral infections
- Difficulty wearing dentures

Low saliva levels raise the chance of cavities because acids stay on the teeth longer.
Gum disease progresses faster when tissues stay dry and inflamed. Oral infections become more common because bacteria spread more easily without saliva to control them.
Taste changes may affect eating habits, and dentures may slip or rub painfully. Many individuals experience a decline in comfort and confidence as dryness affects daily life.
Myths and Misconceptions About Dry Mouth
Misunderstandings about dry mouth often prevent people from addressing the issue early. A few common myths continue circulating, so clear explanations help correct them.
Myth 2 suggests only older adults experience dryness, even though people at many ages can develop it. Midlife simply increases the likelihood.
Myth 3 minimizes dryness as a small inconvenience, even though untreated dryness may cause serious long-term issues.
How to Ease Dry Mouth
@bupadentalcareuk Having issues with dry mouth? It’s not always what you may think, John’s here with some helpful tips. 🙌🏼 #drymouth #drymouthproblems ♬ original sound – Bupa Dental Care UK
Many strategies exist for managing dryness, ranging from simple daily habits to medical treatments. Each category offers helpful steps that people can adopt gradually.
At-Home Remedies and Lifestyle Changes
- Frequent sips of water
- Sugar-free gum
- Xylitol lozenges
- Reduced caffeine and alcohol
- Tobacco avoidance
- Bedroom humidifier
Regular small sips of water support moisture without overwhelming the stomach. Sugar-free gum stimulates saliva and keeps the mouth more comfortable.
Xylitol lozenges encourage moisture and discourage bacterial growth.
Reducing alcohol, caffeine, and tobacco helps maintain stable hydration throughout the day. A humidifier raises moisture in bedroom air and reduces nighttime dryness.
Oral Hygiene Adjustments
Oral care plays a significant role in maintaining comfort and protecting teeth during dry mouth.

- Fluoride toothpaste
- SLS-free toothpaste for sensitive users
- Alcohol-free mouthwash designed for dryness
- Consistent brushing and flossing
- Professional guidance when dryness persists
Fluoride toothpaste strengthens enamel and protects against cavities.
People sensitive to SLS can switch to a gentler formula. Alcohol-free mouthwashes ease irritation while supporting oral hygiene. Regular brushing and flossing reduce buildup and prevent gum complications.
Professional care at dental clinics like TannlegeTeam provides advice when dryness becomes difficult to manage alone.
Medical and Dental Interventions
When dryness continues despite home care, more advanced solutions may be necessary.
- Medication adjustments
- Saliva substitute sprays or gels
- Prescription saliva stimulants
- Regular monitoring by dental professionals
Conversations with medical providers sometimes uncover medication changes that reduce dryness. Saliva substitutes offer instant relief and help keep tissues moist.
Prescription treatments stimulate gland activity in suitable patients. Regular checkups ensure that dryness does not lead to complications.
When to See a Dentist or Specialist

Professional evaluation becomes important when dryness persists or becomes painful.
- Persistent soreness
- Oral infections
- Trouble swallowing
- Significant difficulty speaking
- Ongoing dryness despite home care
Persistent dryness that does not improve with at-home strategies requires expert assessment.
Signs of infection, increasing discomfort, or swallowing difficulty deserve prompt attention.
Some individuals benefit from specialized testing to evaluate salivary gland function.
Clinics focusing on oral medicine offer detailed evaluations and targeted treatment plans when dryness becomes severe.
Summary
Dry mouth after forty is common but manageable with consistent care.
Identifying root causes and improving daily oral habits reduces discomfort and long-term dental risks.
Early attention improves comfort, confidence, and overall oral health.
Related Posts:
- What Are the Common Signs and Symptoms of Vape Rashes?
- Histamine and Menopause - Can Antihistamines Help…
- HRT And Me: I Finally Feel Good – But Why Am I…
- Fluid Retention vs. Edema: The Differences and Why…
- Why the UK’s Ban on Disposable Vapes Is a Positive Step
- Should Beauty Pros Be Ready for the Unexpected?…








